Insight
While the NSW School study of 18 pupils suggests that the risk of Covid19 spread from reopening schools is small, a much more comprehensive study of 661 students, teachers, parents and siblings from a school at the centre of the first outbreak of Covid19 in France suggests substantial spreading of the virus in a high school occurred there.
As promised, the government yesterday released its research justifying the opening of schools in NSW. It looked at 18 confirmed Covid19 cases in NSW primary and high schools. Of those 18 cases, there were two documented transmissions within the school environment, to a further two school students, out of a possible 863 close contacts (around a third of whom were tested for the virus or for antibodies – the rest were isolated for two weeks in case they became sick). All but one of the primary school cases, and around half of the high school cases were found after 23 March – the Monday when the vast majority of NSW school students started learning from home.
The conclusion in the study is that that spread of COVID-19 within NSW schools has been very limited. This conclusion is reached more by looking at 2 new cases as a proportion of a possible 863 close contacts (a very small proportion) rather than looking at 2 confirmed cases out of 18 students (which is a transmission rate of more than 10%, lower than the average for this virus, but not zero).
Our detailed investigation of COVID-19 cases in 15 NSW primary and high schools found only two secondary cases, both in students. This was despite initial cases occurring in 9 students (including two students in two schools) and 9 teachers. Very detailed follow-up, including additional testing for the presence of the virus and for antibodies to the
virus, occurred in a proportion of the total 863 close contacts identified from the school setting….…The findings from this detailed investigation are preliminary. However, they do suggest that spread of COVID-19 within NSW schools has been very limited.
This conclusion in NSW contrasts with a considerably larger study from France.
The comprehensive study (not yet peer reviewed) has just been released on a school from one of the first clusters in France – a school in Crépy-en Valois, a town of 15,000 where a 60 year old teacher was the first local Covid19 fatality in France in February.
On 24 February, a patient from the Oise department, north of Paris, was admitted to hospital in Paris in a critical condition and diagnosed with SARS-CoV-2 infection. He died on 25 February. The ensuing epidemiological investigation led to the identification of a cluster of COVID-19 that involved a high school in the Oise department. Case investigation and contact tracing identified two cases in a high school and who had symptoms consistent with COVID19 on 2 February 2020, suggesting circulation of the virus in the Oise department since the end of January 2020.
As a follow-up to the initial case investigation and contact tracing, a retrospective closed cohort study was conducted in the high school. Between 30 March and 4 April, all pupils, as well as teachers and non-teaching staff (administrative, cleaners, catering) from the high school were invited to participate in the investigation. Since most pupils were minor, at least one parent was invited to participate in the study, to provide informed consent for their child and for any of the other children over the age of 5 years in the household enrolled in the study.
The school had 1,132 pupils and 130 teaching staff. Of those, 326 agreed to participate in the study. A further 345 parents and siblings of students were included, which, with a few excluded as blood samples were unusable, led to 661 people in the study. All were tested for Sars-Cov2 antibodies, and 25.9% were positive (Infection Attack Rate (IAR) of 25.9%). At the same time, blood from donors in a nearby town was tested, and the IAR for them was much smaller, at 3%.
There was no difference in IAR between males and females, while IAR was highest (40.0%) in the 15-17 years age group. The IAR was higher in the high school group (38.3% 43.4%, and 59.3% for pupils, teachers, and school staff, respectively) than in parents and siblings (11.4% and 10.2%, respectively).
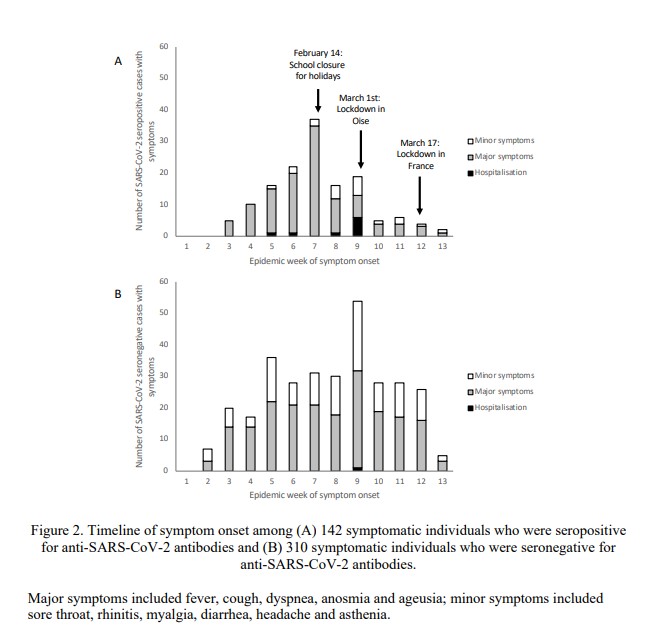
Among those with confirmed infection, the number of new cases dropped dramatically after week 7 [measured by reported symptoms], corresponding to the beginning of the school holidays, and again after local confinement measures were introduced in the Oise department.
The NSW study includes contact tracing, where the French study looks retrospectively at overall infection rates to draw conclusions. But the difference between infections among all attendees at the school – 41% IAR, and those associated with the school – 11% IAR – suggests that the French school was a cluster in its own right, rather than just being a part of a community spreading the disease, leading to material spreading of the virus within the school population. And for teachers and staff, they were more likely to be infected than school students.
There is considerable evidence that children are less likely to become sick with Covid19 than adults. There is reasonable evidence that they are less likely to be infected, and that if they are infected they are less likely to spread it. But the risk is clearly greater than zero, and I haven’t seen any evidence in any of the studies that lead to this conclusion:
Prime Minister Scott Morrison says the government’s medical advice confirms social distancing requirements do not apply to classrooms, clearing the way for students to return to school.
Most of the time, Australia’s actions in this pandemic have been based on looking around the world for good evidence. The evidence from the school in France suggests strongly that schools can be the source of infections for students and teachers alike, and that closing the schools, before any lockdown of the town, reduced the spread of infections within the school.
It seems odd that the evidence being relied on for a decision affecting more than a million school students (and their teachers) is based on 18 students from one state in Australia.
Link
This article about superspreading events, and what they might tell us about Covid19 is fascinating, and thought-provoking. The author points out that he is an interested amateur, but nonetheless, one who has researched super-spreading events across all the public information he could find, to see if they tell us anything more about how Covid19 spreads in practice:
Gaining such an understanding is absolutely critical to the task of tailoring emerging public-health measures and workplace policies, because the process of policy optimization depends entirely on which mechanism (if any) is dominant:
If large droplets are found to be a dominant mode of transmission, then the expanded use of masks and social distancing is critical, because the threat will be understood as emerging from the ballistic droplet flight connected to sneezing, coughing, and laboured breathing. We would also be urged to speak softly, avoid “coughing, blowing and sneezing,” or exhibiting any kind of agitated respiratory state in public, and angle their mouths downward when speaking.
If lingering clouds of tiny aerosol droplets are found to be a dominant mode of transmission, on the other hand, then the focus on sneeze ballistics and the precise geometric delineation of social distancing protocols become somewhat less important—since particles that remain indefinitely suspended in an airborne state can travel over large distances through the normal processes of natural convection and gas diffusion. In this case, we would need to prioritize the use of outdoor spaces (where aerosols are more quickly swept away) and improve the ventilation of indoor spaces.
If contaminated surfaces are found to be a dominant mode of transmission, then we would need to continue, and even expand, our current practice of fastidiously washing hands following contact with store-bought items and other outside surfaces; as well as wiping down delivered items with bleach solution or other disinfectants.
After looking at all the 54 superspreader events (SSEs) found in the public record, the conclusion the author finds is that the first mode of transmission is dominant – and that means avoiding indoor places with intense conversations and other interactions.
When do COVID-19 SSEs happen? Based on the list I’ve assembled, the short answer is: Wherever and whenever people are up in each other’s faces, laughing, shouting, cheering, sobbing, singing, greeting, and praying. You don’t have to be a 19th-century German bacteriologist or MIT expert in mucosalivary ballistics to understand what this tells us about the most likely mode of transmission.
It’s worth scanning all the myriad forms of common human activity that aren’t represented among these listed SSEs: watching movies in a theater, being on a train or bus, attending theater, opera, or symphony (these latter activities may seem like rarified examples, but they are important once you take stock of all those wealthy infectees who got sick in March, and consider that New York City is a major COVID-19 hot spot). These are activities where people often find themselves surrounded by strangers in densely packed rooms—as with all those above-described SSEs—but, crucially, where attendees also are expected to sit still and talk in hushed tones.
Life Glimpses
On a weekend when some beaches reopened a little, it did seem to me that there were more people outside than there had been the previous weekend. The weather was absolutely fantastic, so it was hard to resist, nevertheless I think the general population patience is starting to wear thin for being serious about lockdown (as new cases of Covid19 continue to fall). I’m one of those relaxing slightly; I visited my mother on the weekend (keeping 1.5m away from her at all times), which I had refused to do for the previous three weeks.
It’s going to have to happen again, though, she needs IT support from someone in this house, and I’m not sure how feasible that is going to be over skype.
Bit of Beauty
The beautiful sunny autumn days here in Sydney are gradually becoming more wintry (as much as it gets in Sydney), but that does make the sunsets more interesting as we get clouds to add into the mix. I couldn’t capture the colours properly on my old iPhone, but they were fabulous.


Hi Jennifer
I both enjoy and value your daily insights re CV-19. You must be putting in a ton of research to find, sieve through and interpret so much interesting material. Well done and thanks.
Thanks, Jennifer. It is an important subject and it is worth looking at different perspectives. I agree that 18 people doesn’t sound like a lot but it was not a sample. They have investigated every known case in the NSW schools system. My ignorant/optimistic perspective is not based on looking at 2 cases of infected children out of 18 cases but looking at only 2 cases of transmission during six weeks of schooling across NSW. And, yes, the risk is greater than zero so we need to be clear on what the benefits are to outweigh that risk.
Thanks Martin, I discovered this article after I completed the post, about NZ’s biggest cluster – the analysis is not as comprehensive as NSW, but it is hard to avoid the conclusion that students, teachers and parents were infecting each other.
The reflections are far too clever for me. It gives me great pleasure to let you know
that on front page of The New York Times of today 27.4.20 (I subscribe to the paper edition)
“2 Countries blaze a trail to quell the pandemic” a long article on Australia and New Zealand.
Lovely that you visited Jean, here the distance to be kept is 2 meters, so I suppose one shouts louder.
I think your old iPhone did wonders, may be you could make the photo poster size.
love Marta
Hi Jennifer, some great reading in the links you posted today. Re the NSW study: I think there are some serious flaws in the methodology, but that doesnt necessarily invalidate their conclusion – just that the study hasnt convinced me that their conclusion is correct. Re the French study: I think it confirms that students are less likely to pass onto adults rather than vice versa (only 11%/10% of parents/siblings infected, which I think is highly significant given they are living together). Also confirms contact between adults in school setting more of a risk (non-teaching staff 59% versus teaching staff 43%). 17% asymptomatic is interestingly low compared with other studies, but this may be sample bias? Conclusions around loss of taste/loss of smell being best predictors for the disease should factor into our recommendations on who should come forward for testing. Re the NZ cluster: while obviously lots of transmission between teachers/parents/students, it is not clear that this all happened in a school setting. There was a social evening where many COVID-positive were present, which links into your other article on SSEs. Many teachers/parents could have picked up here and subsequently transmitted to students, with possibly only minimal transmission at the school itself. Personally, I’ll feel much more comfortable about sending my kids back to school if our numbers in NSW stay low for the next few weeks, and the sentinel testing gets rolled out ASAP.
Cheers, Karen
And re SSEs – while I agree that many of the behaviours that lead to spreading are present in schools, there are some things that are missing – alcohol (a great remover of inhibitions, thus more touching, etc and more spitting while talking!), the communal cup or equivalent at religious events (i.e a shared object), kissing and hugging greetings (while some older friendship groups may greet each other this way, most dont)
Stumbled across this site today – not sure if you have discovered it. An evidence summary of the paediatric literature on COVID, written by a group of Aust and NZ paediatricians.
https://dontforgetthebubbles.com/evidence-summary-paediatric-covid-19-literature/