Australia has had very little Covid19 compared with the rest of the world, due to very strict border controls and lockdowns. But with the rest of the world opening up as their populations are increasingly vaccinated, how does Australia do the same? I look at some initial modelling from the Burnet Institute. My key takeaways? The better the vaccine efficacy (particularly against any form of infection and transmission) the more we can open up without serious Covid19 disease. And waiting until a reasonable proportion of the population is vaccinated (say 40%) makes a real difference to the incidence of severe disease and death.
The Burnet Institute has done some modelling of the impact of easing Covid19 restrictions in Victoria, using a range of assumptions (about both vaccination uptake and effectiveness). They’ve also released a spreadsheet so that you can see the effect of different assumptions. In the UK, a number of similar institutions have done the same thing, summarised by the UK government here. The UK Covid19 Actuaries Response Group has analysed the three main studies in the UK, which shows the wide range of justifiable assumptions.
Here in Australia, the question we should be asking is what the trigger points should be to start easing open our borders. The Burnet Institute modelling, which was originally built to help make decisions about last year’s Melbourne lockdown, gives an initial view of what the outcomes might be from opening borders at different levels of population vaccination. What they have published enables a look at the outcomes of a wide range of justifiable assumptions.
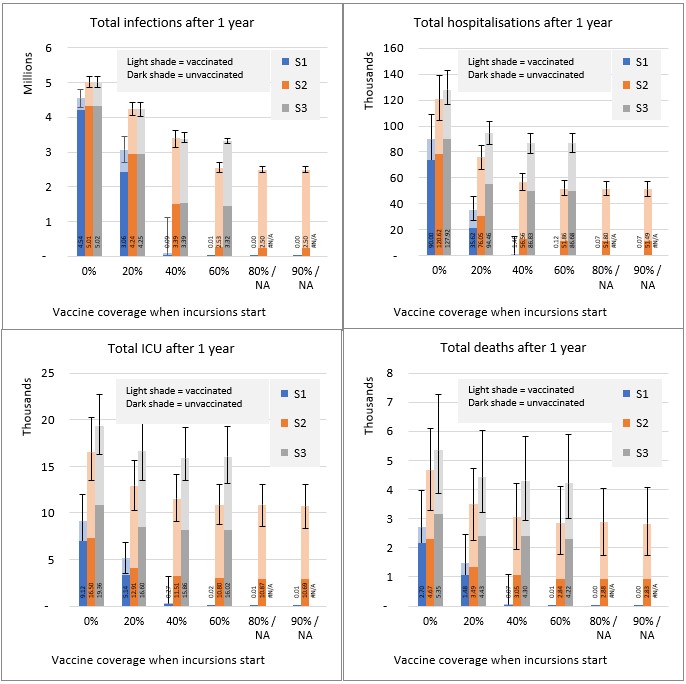
What trade offs are we willing to make in illnesses, hospitalisations and (sadly) deaths for the benefits of letting people into Australia with less or no quarantine? Does it make a difference if the people are not vaccinated? The Burnet Institute underlying scenario looks at the Victorian population. It has one case per day being seeded into the community, starting at different points of population vaccination coverage, and either 150,000 or 250,000 doses of vaccine given in the community per week (last week Victorians received around 225,000 doses). The scenarios do not currently include any major public health response to gain control of outbreaks. On detection of the first case, the model assumes symptomatic testing increases (isolation of positive cases continues), masks become recommended but not mandatory, and contact tracing continues but only up to 250 diagnoses per day. Hence the projections represent very little public health response – adding in public health responses would improve them. The results shown are the total incidence of Covid19 cases, symptomatic infection, hospitalisations, ICU admissions and deaths) for the 12 months after cases are seeded into the community.
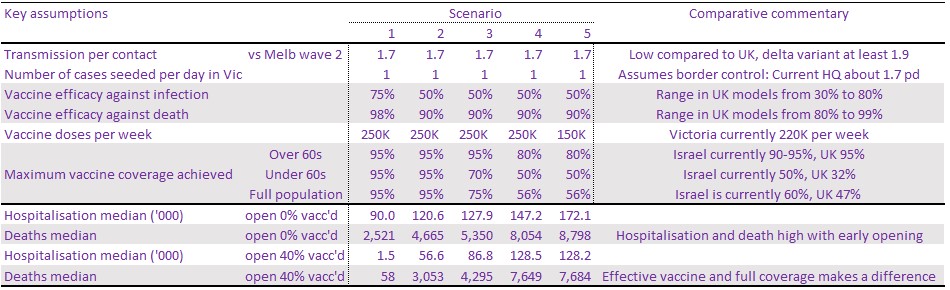
The Burnet Institute gives the ability to try quite a few different assumptions. I’ve shown the assumptions I’ve chosen and results for five scenarios below:
There are around 6.6 million people in Victoria, just over a quarter of the Australian population. While the model looks at Victoria, the pattern for the rest of Australia (and probably NZ and other countries in Asia that have had very little Covid19 to date) is likely to be pretty similar in outcomes for similar assumptions.
The scenarios start with the most optimistic from the available assumptions, and then work back from there. Scenario 1 is an optimistic view of how effective the vaccine is likely to be, particularly against transmission, as well as assuming that 95% of the whole population is currently vaccinated. Scenario 2 reduces vaccine efficacy to what seems more likely (around the mid point of the various UK scenarios, noting that Astra Zeneca is generally slightly less effective at each stage of infection, symptoms, hospitalisation, ICU and death). And then the remaining scenarios look at changes in the vaccine rollout – reducing the ultimate level in two stages to 95%/75% (over 60s and under 60s) then 80%/50%, and then slowing the rollout down to be slightly slower than currently in Australia. For comparison, Israel’s current vaccine coverage is 90-95%/50%, and the UK is 95%/32%. The graphs below show the results for the first three scenarios.
A reminder that all these numbers are for Victoria only, which is 25% of Australia, so to get to the whole of Australia, multiply by 4.
This model enables almost too many parameters, and shows again, just how hard it is to model an exponential situation with uncertain parameters. My key takeaways are
- Even with everything we know now about vaccine efficacy, small changes, particularly in efficacy against transmission can make a big difference to the ultimate outcome
- On all scenarios (including a very effective vaccine), opening the borders before we reach around 40% vaccination will cause significant illness and death
- Aiming for 100% population coverage of the vaccine substantially reduces illness and death over the next 12 months, even if we open up before then
- Based on what we currently know about the vaccines, opening up Australia, even after substantial vaccine coverage, is likely to lead to thousands of deaths from Covid19, unless we maintain some degree of public health measures (social distancing, working from home, etc).
Unless a very optimistic view of the effectiveness of vaccinations is true, particularly of their effectiveness against spread, opening up the Australian economy to overseas visitors without some form of testing and quarantine is very likely to lead to significant hospitalisation and deaths from Covid19. Public health measures are likely to be here to stay, unless Australians have a very big change in risk appetite.
For comparison, in 2019, 4,075 people in Victoria died of diseases of the respiratory system, including 1,135 from influenza and pneumonia and 2,006 from chronic lower respiratory diseases. In total 43,944 people died in Victoria in 2019. In Victoria to date, 820 people have died from Covid19.
Thanks to frequent commenters here Karen, Kirsten and Richard for some suggestions about how to write this analysis.
Links
This analysis looks at vaccination rates and projects when Australia is likely to reach what they describe as herd immunity – 70% full vaccination of the population:
In summary, Coolabah’s research estimates the duration of the three different components of Australia’s journey to reaching herd immunity based on empirically observed experiences around the rest of the world. The first phase one roll-out takes about 114 days to ensuring 80% of the adult population gets their initial dose. The slower phase two process takes another 41 days to reach 90.8% of adult population (or equivalently 70% of total population). The final phase three process requires 90 days to secure 70% of total population having been fully vaccinated. This implies about 245 days from the time of writing, and suggests that Australia should get to herd immunity somewhere between mid January 2022 and late February 2022.
As NSW has its own outbreak of this variant, the latest on the delta variant from Kai Kupferschmidt and Meredith Wadman in Science Magazine.
Research by Public Health England underscores Delta’s ability to spread. Compared with Alpha, which appeared in the United Kingdom in 2020, “You’re getting estimates of 50% or 100% more transmission,” says Adam Kucharski, a modeler at the London School of Hygiene & Tropical Medicine.
But Kucharski says reduced protection from vaccines may play a role as well. Data from England and Scotland indicate that both the Pfizer-BioNTech and AstraZeneca vaccines offer slightly less protection against symptomatic infections from the new variant than from Alpha. People who have received just one shot of vaccine—as many U.K. residents have—are especially vulnerable. (Two doses of either vaccine still offer the same high level of protection from hospitalization from Delta.) How well the many other vaccines now in use around the world protect against it is unclear, and there are few data on the protection resulting from a prior bout of COVID-19.
If Alpha really is approximately 50% more transmissible than the wild type strain, and Delta is 50% more transmissible again than Alpha, we’re talking about a virus that’s more than twice as transmissible as the initial strain
Ed Yong (who recently won the Pulitzer prize for his pandemic reporting) in the Atlantic (from the US where they are well ahead of Australia on vaccination) looks at the balance between collective action and individual action in a very individualistic country – who bears the residual risk once most vaccination has taken place, particularly for those who are well off?
Collective action is not impossible for a highly individualistic country; after all, a majority of Americans used and supported masks. But such action erodes in the absence of leadership…
…Rather than ushering in an era of flexibility, the CDC has arguably triggered a chain of buck-passing, wherein responsibility for one’s health is once again shunted all the way back to individuals. “Often, Let everyone decide for themselves is the easiest policy decision to make, but it’s a decision that facilitates spread of COVID in vulnerable communities,” Julia Raifman, a health-policy researcher at Boston University, told me.
Life glimpses
Since my last post, I’ve been to the South Coast of NSW – instead of Victoria where I had been planning to be before there was another Covid19 outbreak in Melbourne. And now we have an outbreak in NSW, and I’m writing this on our first full day of lockdown in Greater Sydney. It’s a beautiful winter day, and there are lots of people out walking and riding bikes, which is lovely to see. In an amusing development, toilet paper was on sale at our local supermarket yesterday, so hopefully that means people have finally realised that panic buying is not necessary.
I’ve also been following vaccinations in people I know well enough to ask. So far everyone I have talked to has sought out a vaccination if they can, even to the point of inconveniencing themselves. But among the people I talk to, I don’t know anyone who would lose income from going and getting vaccinated (either at Sydney Olympic Park or their local GP), or having to take a day off with side effects.
Bit of beauty
On my trip to the South Coast (instead of Melbourne), I came across this beautiful piece of sandstone. A real geology lesson.